Introduction to Chronic Urticaria
Chronic urticaria, often referred to as hives, is a condition marked by the recurrent appearance of itchy welts on the skin. These welts, or hives, can vary in size and may appear anywhere on the body. The condition becomes chronic when these symptoms persist for six weeks or longer, distinguishing it from acute urticaria, which typically resolves within a shorter period. While the exact cause of chronic urticaria remains elusive in many cases, it is generally understood to be a complex interplay of factors.
Symptoms of chronic urticaria include the sudden onset of raised, red or skin-colored welts, which are often accompanied by itching. These welts can change shape, move around, and disappear and reappear over the course of minutes or hours. In severe cases, the swelling can extend below the skin, causing angioedema, which may affect the face, lips, tongue, throat, or other areas of the body, potentially leading to difficulty in breathing and swallowing.
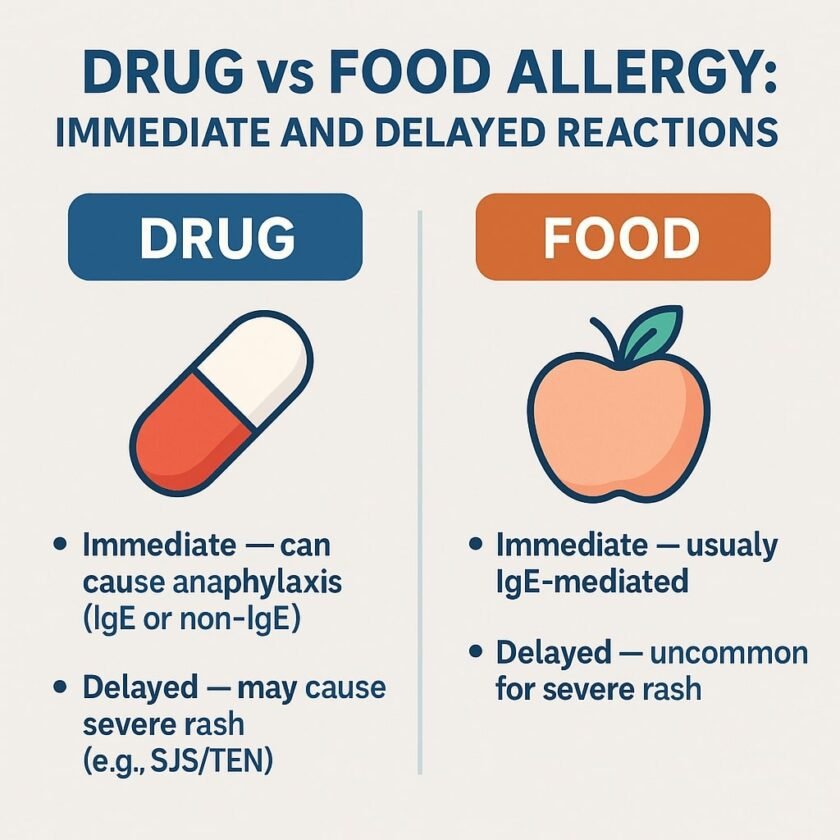
Potential triggers for chronic urticaria can be diverse, ranging from food allergens and medications to environmental factors such as heat, cold, pressure, and stress. However, in a significant number of cases, the exact cause remains unidentified, a condition known as chronic idiopathic urticaria. This variability in triggers and the chronic nature of the condition can significantly impact the quality of life for those affected.
The duration of chronic urticaria can also be unpredictable. For some individuals, the condition may resolve within months, while others may experience symptoms for years. This unpredictability underscores the importance of comprehensive management strategies, which may include lifestyle adjustments, avoidance of known triggers, and the use of medications to control symptoms.
Understanding the intricacies of chronic urticaria is crucial, as it sets the foundation for exploring its potential links to other health issues, such as autoimmune disorders and hormonal imbalances. By delving into these connections, we aim to provide a more holistic view of the condition and potential pathways for more effective management and treatment.
Autoimmune Thyroiditis and Urticaria
Autoimmune thyroiditis, commonly referred to as Hashimoto’s thyroiditis, has garnered significant attention in medical research due to its potential link with chronic urticaria. Chronic urticaria, characterized by persistent hives, shares a complex relationship with various autoimmune disorders, including Hashimoto’s thyroiditis. Scientific evidence suggests that an autoimmune mechanism may underpin both conditions, possibly through shared pathophysiological pathways.
In Hashimoto’s thyroiditis, the immune system mistakenly attacks the thyroid gland, leading to hypothyroidism. This autoimmune assault results in the production of autoantibodies, which can trigger systemic inflammation. Chronic urticaria, on the other hand, is marked by recurrent episodes of hives and can be exacerbated by immune dysregulation. The presence of thyroid autoantibodies, such as anti-thyroperoxidase (TPO) and anti-thyroglobulin, has been observed in a notable percentage of patients with chronic urticaria, suggesting a potential immunological link.
Several case studies and clinical trials have shed light on the association between these two conditions. For instance, a study published in the Journal of the American Academy of Dermatology found that patients with chronic urticaria had a higher prevalence of thyroid autoantibodies compared to the general population. This observation supports the hypothesis that autoimmune thyroiditis may contribute to the pathogenesis of chronic urticaria through immune-mediated mechanisms.
Recognizing the potential connection between chronic urticaria and autoimmune thyroiditis is crucial for clinical practice. Thyroid function tests, including measurements of thyroid-stimulating hormone (TSH), free thyroxine (FT4), and the aforementioned autoantibodies, are essential in the diagnostic workup of patients presenting with chronic urticaria. Early detection of thyroid dysfunction can lead to appropriate management, potentially alleviating the severity of urticaria symptoms.
In conclusion, understanding the intricate relationship between autoimmune thyroiditis and chronic urticaria can enhance diagnostic accuracy and therapeutic strategies. Continued research into the immunological interplay between these conditions is essential for improving patient outcomes and developing targeted treatments.
Chronic Urticaria and Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is a prevalent hormonal disorder affecting women of reproductive age, characterized by irregular menstrual cycles, elevated androgen levels, and polycystic ovaries. Emerging research suggests a notable connection between PCOS and chronic urticaria, a condition marked by persistent hives. Hormonal imbalances inherent in PCOS may play a significant role in the development and exacerbation of chronic urticaria.
Several studies have indicated that the hormonal dysregulation in PCOS, particularly an excess of androgens and insulin resistance, can lead to an inflammatory state that may trigger chronic urticaria. Elevated testosterone levels and insulin resistance can increase the production of pro-inflammatory cytokines, which are known to mediate immune responses and contribute to the development of hives. Furthermore, the imbalance in estrogen levels could affect mast cell stability, leading to an increased release of histamine, a primary mediator in urticaria.
One notable study conducted on women with PCOS revealed a higher prevalence of chronic urticaria compared to the general population. The research underscored the importance of considering hormonal evaluations in patients presenting with chronic urticaria, particularly if they exhibit symptoms indicative of PCOS, such as hirsutism, acne, and menstrual irregularities. This connection underscores the need for a multidisciplinary approach in managing chronic urticaria, incorporating both dermatological and endocrinological perspectives.
Evaluating patients with chronic urticaria for underlying PCOS can lead to better-targeted treatments. For instance, addressing insulin resistance through dietary modifications, physical activity, and medications like metformin may alleviate both PCOS symptoms and chronic urticaria. Hormonal therapies that regulate androgen levels may also reduce the incidence and severity of hives, improving the overall quality of life for affected individuals.
The interrelationship between chronic urticaria and PCOS exemplifies the complexity of hormonal and immune system interactions. It highlights the importance of comprehensive patient evaluations to identify underlying conditions that may contribute to chronic urticaria, ultimately leading to more effective and individualized treatment strategies.
Dermatomyositis as a Paraneoplastic Syndrome of Ovarian Cancer
Dermatomyositis is an inflammatory condition marked by muscle weakness and a distinctive skin rash. It is crucial to recognize that dermatomyositis can sometimes act as a paraneoplastic syndrome, indicating the presence of underlying malignancies, such as ovarian cancer. This association underscores the importance of distinguishing dermatomyositis from other dermatological conditions, such as chronic urticaria.
The clinical features of dermatomyositis include a heliotrope rash, which is a violet or dusky discoloration around the eyes, and Gottron’s papules, which are raised, scaly eruptions typically found over the knuckles. Additionally, patients may experience proximal muscle weakness, making it difficult to perform everyday activities such as climbing stairs or lifting objects. These symptoms can often be mistaken for those of chronic urticaria, which primarily presents with red, itchy welts on the skin. However, the presence of muscle weakness and the specific type of rash seen in dermatomyositis are distinguishing factors.
Diagnosing dermatomyositis involves a combination of clinical evaluation, laboratory tests, and imaging studies. Blood tests may reveal elevated levels of muscle enzymes, such as creatine kinase, and the presence of autoantibodies. Electromyography (EMG) and muscle biopsy can also aid in confirming the diagnosis. Given the potential link between dermatomyositis and malignancies, cancer screening becomes a crucial component of the diagnostic process. For female patients, this includes thorough gynecological examinations and imaging studies such as pelvic ultrasound or CT scans to assess for ovarian cancer.
The role of cancer screening cannot be overstated. Early detection of ovarian cancer in patients presenting with dermatomyositis can significantly improve patient outcomes. Physicians should maintain a high index of suspicion and promptly initiate appropriate diagnostic strategies when encountering patients with suspicious skin rashes and muscle weakness. By distinguishing dermatomyositis from chronic urticaria and recognizing its potential as a paraneoplastic syndrome, healthcare providers can ensure timely and effective intervention.
Differentiating Between Urticaria and Dermatomyositis
Accurate diagnosis is crucial when differentiating between urticaria and dermatomyositis, as each condition demands a distinct treatment approach. Urticaria, commonly known as hives, is characterized by the sudden onset of raised, itchy welts on the skin. These welts can vary in size and often migrate across different parts of the body. Urticaria typically resolves within 24 hours, though chronic cases can persist for six weeks or longer.
In contrast, dermatomyositis is a systemic inflammatory disease primarily affecting the skin and muscles. Unlike the transient nature of urticaria, dermatomyositis presents with persistent symptoms. Key dermatological features include a heliotrope rash, which manifests as a violet or dusky discoloration around the eyelids, and Gottron’s papules, which are raised, scaly bumps found over the knuckles. Additionally, patients with dermatomyositis often experience muscle weakness, particularly in the proximal muscles, making everyday activities like climbing stairs or lifting objects challenging.
Diagnostic tests further aid in distinguishing between these two conditions. For urticaria, allergen exposure and physical triggers like heat or stress are evaluated, and blood tests may reveal elevated levels of IgE antibodies. On the other hand, diagnosing dermatomyositis involves more comprehensive testing. Elevated muscle enzymes such as creatine kinase, electromyography (EMG) findings, and muscle biopsy results are indicative of muscle inflammation. Furthermore, autoantibodies such as anti-Mi-2 and anti-Jo-1 are often present in individuals with dermatomyositis.
Given the overlapping symptoms of skin manifestations, misdiagnosis can occur, leading to inappropriate treatments. Understanding the distinct clinical presentations and employing specific diagnostic tests are essential steps in ensuring that patients receive the correct diagnosis and management plan. This not only improves patient outcomes but also alleviates the burden of chronic symptoms and potential complications associated with each condition.
Hormonal Hypersensitivity Reactions: Autoimmune Progesterone Dermatitis
Autoimmune progesterone dermatitis (APD) is a rare but significant hypersensitivity reaction to endogenous or exogenous progesterone. This condition predominantly affects women and is characterized by a cyclical eruption of skin lesions that correspond with the menstrual cycle. Clinical presentations of APD can vary, ranging from urticaria, erythema, and eczema-like rashes to more severe manifestations such as vesicles and bullae. These symptoms typically worsen during the luteal phase of the menstrual cycle when progesterone levels peak.
Diagnosing autoimmune progesterone dermatitis presents a unique set of challenges. Due to its rarity and the broad differential diagnoses of skin conditions, APD is often overlooked. A thorough patient history focusing on the timing of symptoms in relation to the menstrual cycle is crucial. Additionally, diagnostic tests such as intradermal progesterone injection tests and hormone assays can aid in confirming the diagnosis. Patch testing with progesterone may also be employed, but it requires careful interpretation due to potential false positives and negatives.
Treatment options for APD are influenced by the severity of the clinical presentation and patient-specific factors. Hormonal therapies, including the use of oral contraceptives to suppress ovulation or gonadotropin-releasing hormone (GnRH) analogs to induce a hypoestrogenic state, have shown efficacy. These treatments aim to reduce progesterone levels and, consequently, alleviate symptoms. In some cases, corticosteroids and antihistamines may be prescribed to manage acute episodes. For patients experiencing severe or refractory symptoms, alternative approaches such as oophorectomy may be considered, although this is typically reserved for extreme cases.
Hormonal fluctuations play a pivotal role in the pathophysiology of autoimmune progesterone dermatitis and other skin conditions. The interplay between hormones and the immune system can exacerbate or trigger dermatological symptoms. Therefore, it is essential for clinicians to consider hormonal hypersensitivity in the differential diagnosis of chronic and cyclical skin conditions. Awareness and understanding of such rare conditions can facilitate timely and accurate diagnosis, leading to more effective management strategies for affected individuals.
Exploring Hormonal Disturbances in Chronic Skin Conditions
Chronic skin conditions, such as urticaria, often present a diagnostic challenge, particularly when they persist despite standard treatments. An emerging area of interest in dermatology is the potential role of hormonal disturbances in the pathogenesis of these conditions. Hormonal imbalances, involving thyroid, adrenal, and sex hormones, may significantly impact skin health, contributing to the chronicity and severity of skin disorders.
Thyroid dysfunction, including both hyperthyroidism and hypothyroidism, is frequently associated with various dermatological manifestations. Hyperthyroidism can exacerbate conditions like chronic urticaria through increased blood flow and heightened immune responses. Conversely, hypothyroidism is linked with dry, rough skin and can also provoke chronic urticaria due to immune dysregulation. Therefore, screening for thyroid function is a crucial step in the workup of patients with persistent skin issues.
Adrenal hormones, particularly cortisol, play a pivotal role in the body’s response to stress and inflammation. Dysregulation of cortisol levels, such as in Cushing’s syndrome or Addison’s disease, can have profound effects on the skin. Elevated cortisol levels may lead to thinning of the skin, easy bruising, and delayed wound healing, while insufficient cortisol can result in hyperpigmentation and chronic inflammation, potentially aggravating conditions like urticaria.
Sex hormones, including estrogen and testosterone, also influence skin health. Estrogen promotes skin hydration and elasticity, while testosterone can increase sebum production, affecting skin texture and potentially leading to acne. Imbalances in these hormones, such as those seen in polycystic ovary syndrome (PCOS) or menopause, can manifest as chronic skin conditions, including urticaria. Hormonal evaluation and management might thus be a beneficial component of a comprehensive treatment plan for chronic skin disorders.
The interrelation between hormonal disturbances and chronic skin conditions underscores the importance of a holistic approach to diagnosis and treatment. Thorough hormonal evaluation, including thyroid, adrenal, and sex hormones, should be considered for patients with unexplained chronic skin issues. This comprehensive approach may uncover underlying hormonal imbalances, offering new avenues for effective management and improving patient outcomes.
Conclusion: Integrating Dermatology and Endocrinology for Better Patient Outcomes
In our exploration of chronic urticaria, autoimmune disorders, and hormonal imbalances, it has become evident that the relationship between these conditions is both intricate and significant. Chronic urticaria, often dismissed as a simple dermatological issue, frequently has roots in deeper systemic disorders, including autoimmune diseases and hormonal disruptions. Recognizing these links is crucial for effective patient management and treatment.
Autoimmune disorders, such as thyroid disease, lupus, and rheumatoid arthritis, have been shown to exacerbate or even trigger chronic urticaria. Similarly, hormonal imbalances, particularly those involving the thyroid and adrenal glands, can influence the onset and severity of skin conditions. These factors underscore the necessity for healthcare providers to adopt a holistic, multidisciplinary approach when diagnosing and treating patients with chronic urticaria.
Integrating dermatology and endocrinology can lead to more comprehensive patient care. Dermatologists should consider screening for underlying autoimmune and hormonal issues in patients presenting with chronic urticaria. Endocrinologists, too, should be vigilant about the dermatological manifestations of endocrine disorders. Collaborative efforts between these specialties can facilitate earlier diagnosis, more targeted treatments, and ultimately, better patient outcomes.
Healthcare providers are encouraged to maintain open lines of communication and to consider collaborative case management. Regular interdisciplinary meetings and shared patient records can enhance the understanding of how these complex conditions interact, fostering a more integrated care model. This approach not only benefits patients by addressing the root causes of their symptoms but also advances the overall field of medical research by highlighting the interconnectedness of bodily systems.
In conclusion, the intersection of dermatology and endocrinology offers a promising pathway to improving the management of chronic urticaria and related conditions. By embracing a multidisciplinary strategy, healthcare providers can offer more detailed diagnoses and personalized treatments, ultimately enhancing the quality of life for those affected by these challenging health issues.

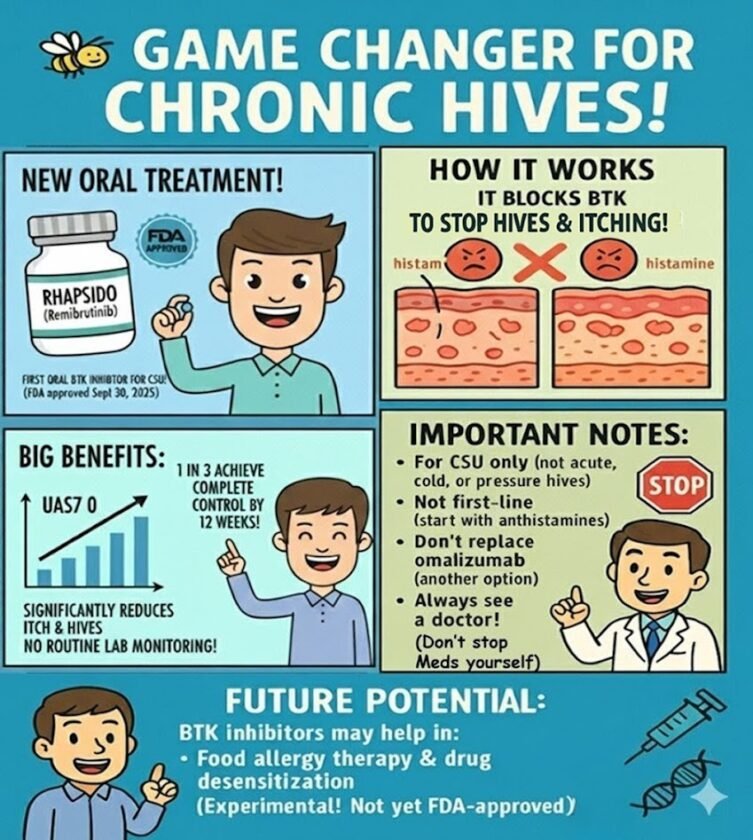
[…] years, patients with chronic spontaneous urticaria (CSU) who didn’t respond to antihistamines had only injections as the next step. On September 30, 2025, […]