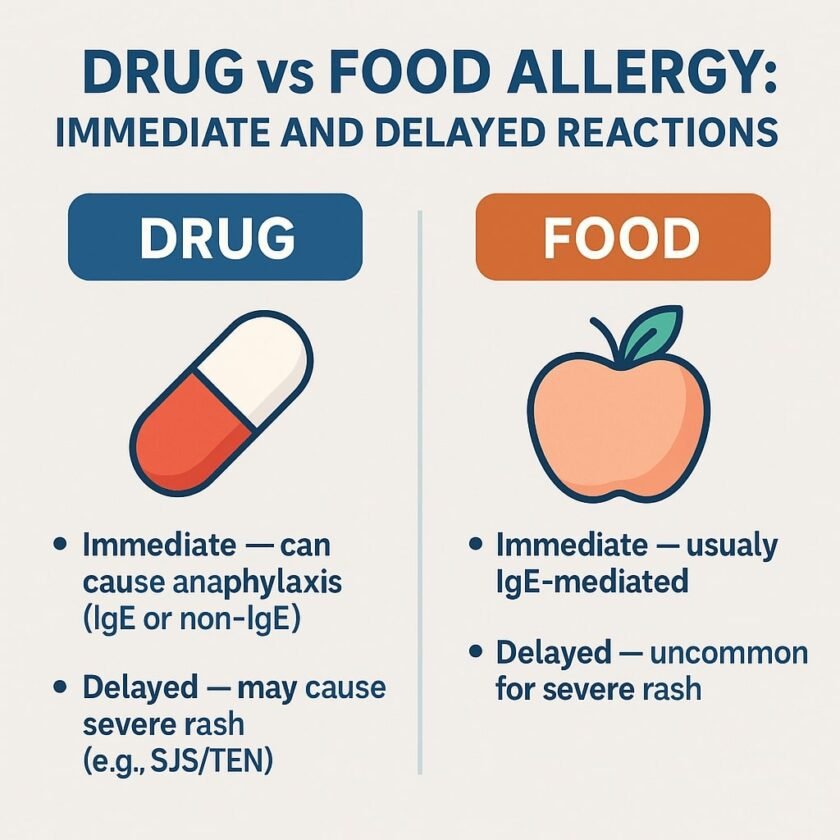
Severe Cutaneous Adverse Reactions (SCARs), such as acute generalized exanthematous pustulosis (AGEP), Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), and Stevens-Johnson Syndrome (SJS), are among the most feared drug-related complications. These conditions can result in devastating outcomes, and the conventional approach to managing SCARs emphasizes strict avoidance of the suspected culprit drug to prevent potentially fatal recurrences. But is avoidance always the only path forward? Could there be room for a more nuanced strategy in specific cases?
Not All SCARs Are Created Equal
SCARs represent a spectrum of disorders, varying widely in severity, organ involvement, and long-term outcomes. For instance:
- AGEP often resolves quickly once the drug is discontinued, with limited systemic involvement.
- DRESS can range from mild presentations to severe cases with life-threatening organ damage, such as liver failure.
- SJS/TEN involves extensive skin and mucosal damage, posing a high risk of mortality and long-term complications.
Given this variability, the question arises: Should every SCAR automatically preclude future use of the suspected drug, or could certain cases warrant a more tailored approach, such as a cautious rechallenge?
Rationale for Drug Challenge in SCARs
Although SCARs are severe, not all suspected drugs on the list are the actual culprits. Evidence shows that most patients are allergic to only one or two drugs in a single episode. Avoiding all potential suspects without discrimination can complicate future management of the patient. This practice can leave patients with limited effective drug options, and in some cases, there may be no alternative therapies for their condition. A carefully planned drug rechallenge can help identify safe options, preserving vital treatments and improving patient outcomes.
Revisiting Rechallenge: When and How?
1. Mild DRESS or AGEP Without Severe Complications
For cases like AGEP or mild DRESS without significant organ damage, a graded drug challenge may be feasible. This involves starting with a very low dose of the suspected drug under close monitoring and gradually increasing the dosage. This strategy can confirm or refute the drug’s role in the initial reaction, enabling patients to use essential medications they may not actually be allergic to.
2. Cases Where Avoidance Is Not Feasible
In conditions like tuberculosis or HIV, where the drugs implicated in SCARs may be irreplaceable, diagnostic tools can guide decision-making:
- In Vitro Tests: Tools like the Enzyme-Linked ImmunoSpot (ELISpot) assay, which measures drug-specific T-cell responses, can assess drug causality.
- ALDEN Score: Drugs with a low ALDEN score may be candidates for rechallenge if necessary, while those with high scores should generally be avoided.
When a rechallenge is required, it should follow these principles:
- Gradual escalation: Start with a very small dose and increase incrementally.
- Controlled environment: Perform the rechallenge in a medical setting equipped with resuscitation equipment.
- Immediate intervention: Be prepared to act promptly if a hypersensitivity reaction occurs. Studies from resource-limited settings, such as South Africa, have shown that early high-dose intravenous corticosteroids can effectively halt reactions during rechallenges of anti-tuberculosis drugs.
Expanding Diagnostic Tools: A Comprehensive Approach
Advances in diagnostic tools are broadening the scope of SCAR management:
- In Vivo Testing: Patch and intradermal tests provide insights into drug hypersensitivity. Patch tests are safer and suitable for most cases, while intradermal tests carry higher risks and should be reserved for select patients.
- In Vitro Testing: Tests like Lymphocyte Transformation Test (LTT) and IFN-gamma ELISpot assays are particularly valuable:
- LTT is most effective for drugs with an ALDEN score below 4, as these are less likely to be the true culprit. Prioritizing these drugs minimizes the risk of severe reactions.
- Combining in vivo and in vitro tests enhances diagnostic accuracy.
- HLA Typing: Identifying genetic predispositions to drug hypersensitivity, such as HLA-B*57:01 for abacavir hypersensitivity syndrome, helps confirm the need for avoidance in known reactions.
Incorporating Predictive Models
Integrating tools like the IFN-gamma ELISpot assay with clinical data has enabled the development of predictive models with over 90% specificity for identifying culprit drugs. These models offer actionable insights, guiding clinicians in deciding whether to rechallenge or avoid a drug.
The Role of Shared Decision-Making
Rechallenging a drug in SCAR cases involves balancing risks and benefits through collaborative decision-making. Key factors to consider include:
- The severity and nature of the previous reaction.
- The availability of alternative therapies.
- The patient’s understanding of the potential risks and benefits.
This shared approach ensures that patients are active participants in their care, with decisions tailored to their unique clinical circumstances.
Disclaimer
Drug rechallenges in SCARs should only be performed by specialists. They should be considered only when the suspected drugs are essential for treatment and must always involve informed consent from the patient.
Final Thoughts
Reassessing SCAR management does not diminish the seriousness of these conditions but highlights the importance of personalized care. By combining in vivo and in vitro diagnostics, leveraging predictive models, and applying clinical judgment, we can tailor approaches to balance safety with therapeutic necessity. Strict avoidance will remain the standard in severe cases, but graded challenges may offer new pathways for improving outcomes in less severe presentations or when no alternatives exist.
Have you encountered a case where drug rechallenge was considered for SCARs? Share your thoughts in the comments below. Let’s continue this conversation to help improve outcomes for patients dealing with these challenging conditions.
References
- Wolkenstein P, Chosidow O, Fléchet ML, Robbiola O, Paul M, Dume L, et al. Patch testing in severe cutaneous adverse drug reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Contact Dermatitis. 1996;35(4):234-6.
- Novack DE, Braskett M, Worswick SD, Adler BL. Drug patch testing in Stevens-Johnson syndrome and toxic epidermal necrolysis: a systematic review. Ann Allergy Asthma Immunol. 2023;130(5):628-36.
- Trubiano JA, Strautins K, Redwood AJ, Pavlos R, Konvinse KC, Aung AK, et al. The combined utility of ex vivo IFN-γ release enzyme-linked immunospot assay and in vivo skin testing in patients with antibiotic-associated severe cutaneous adverse reactions. J Allergy Clin Immunol Pract. 2018;6(4):1287-96.
- Porter M, Smith R, Teixeira N, Thwala B, Choshi P, Phillips EJ, et al. First-Line Antituberculosis Drug Challenge Reactions in Drug Reaction With Eosinophilia and Systemic Symptoms Syndrome in an HIV Endemic Setting. J Allergy Clin Immunol Pract. 2024;12(10):2798-808.
- Lehloenya RJ, Isaacs T, Nyika T, Dhana A, Knight L, Veenstra S, Peter J. Early high-dose intravenous corticosteroids rapidly arrest Stevens-Johnson syndrome and drug reaction with eosinophilia and systemic symptoms recurrence on drug re-exposure. J Allergy Clin Immunol Pract. 2021;9(1):582-4.
- Bellón T, Rodríguez-Martín S, Cabañas R, Ramírez E, Lerma V, González-Herrada C, et al. Assessment of drug causality in Stevens-Johnson syndrome/toxic epidermal necrolysis: Concordance between lymphocyte transformation test and ALDEN. Allergy. 2020;75(4).
- Chongpison Y, Sriswasdi S, Buranapraditkun S, Thantiworasit P, Rerknimitr P, Mongkolpathumrat P, et al. IFN-γ ELISpot-enabled machine learning for culprit drug identification in nonimmediate drug hypersensitivity. J Allergy Clin Immunol. 2024;153(1):193-202.
- Sittiwattanawong P, Kantikosum K, Charoenchaipiyakul K, Pootongkam S, Asawanonda P, Kerr SJ, et al. In-vivo and ex-vivo tests for culprit drugs identification in severe cutaneous adverse drugs reactions. J Dermatol.