Educational Content Disclaimer
This article provides educational information about rare immunodeficiency disorders. It is not medical advice and should not replace consultation with qualified healthcare providers. Individual presentations vary, and management should be personalized under medical supervision.
🔗 Why This Matters for Drug Allergy Detective
At Drug Allergy Detective, we focus on helping you understand drug allergies and hypersensitivity reactions. But to truly understand why certain people react to medications differently, we need to explore the immune system’s foundation.
This article explores two rare genetic conditions that represent opposite extremes of immune dysregulation—and understanding them helps us appreciate:
- Why immune balance matters for drug tolerance
- How underlying immune defects can alter drug reaction patterns
- Why certain medications (like JAK inhibitors) can help restore immune equilibrium
- How chronic inflammation or immune deficiency can influence drug hypersensitivity risk
Think of this as “understanding the foundation before we build the house.” When the immune system’s basic signaling is disrupted, everything downstream—including how your body responds to medications—can change.
🌿 Introduction: When the Immune System Loses Its Balance
The human immune system is one of nature’s most remarkable balancing acts. Every day, it works quietly to protect us—strong enough to fight infections, yet restrained enough to avoid attacking our own cells.
But what happens when this delicate balance tips too far to one side?
If the immune system becomes overactive, it can burn itself out, leading to chronic inflammation and autoimmunity. If it becomes too weak, even mild infections can become serious threats.
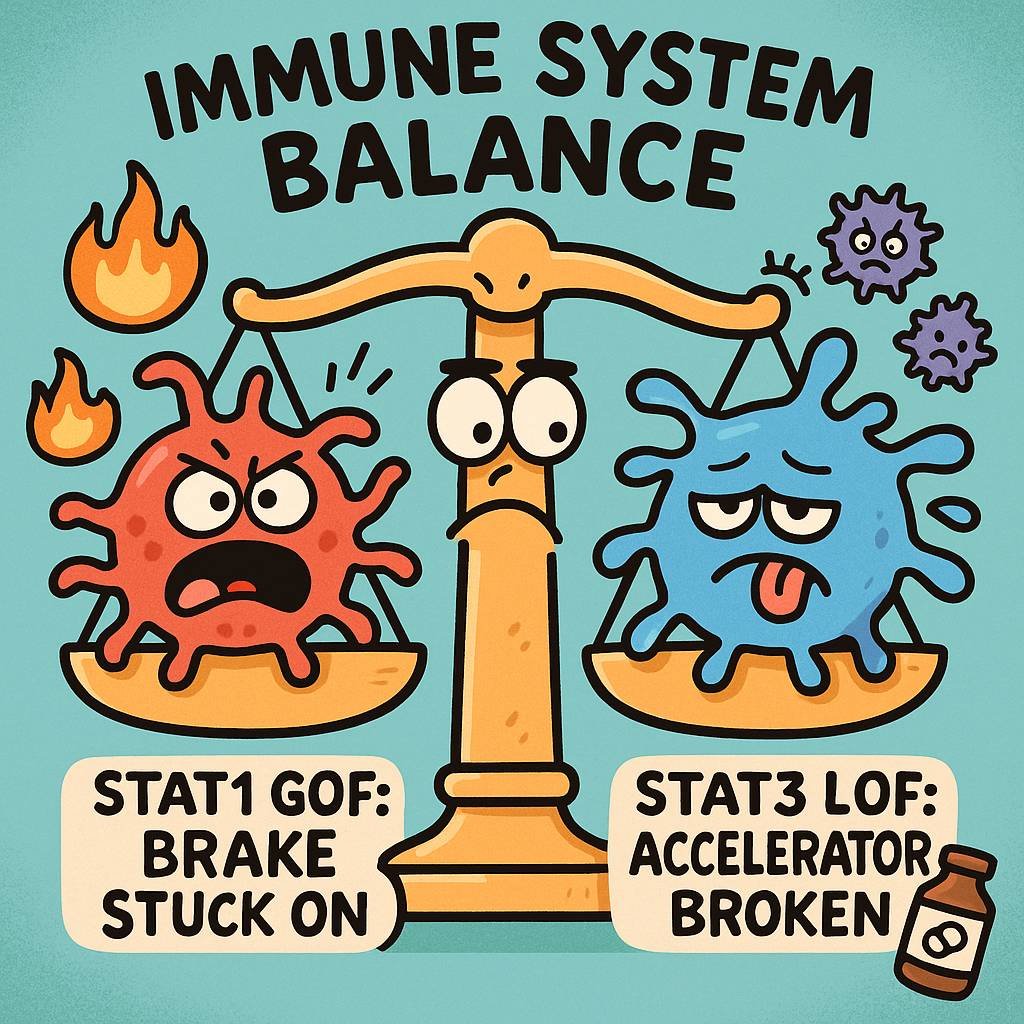
In today’s article, we’ll explore two rare genetic conditions that perfectly illustrate this concept of immune balance gone wrong:
- STAT1 Gain-of-Function (GOF)
- STAT3 Loss-of-Function (LOF)
They act as mirror opposites—one where the “brake” of the immune system is jammed on, and another where the “accelerator” fails to respond. Both can lead to infections, inflammation, and confusion for doctors and patients alike.
By understanding these two disorders, we can appreciate how the immune system maintains equilibrium—and how targeted treatments can help restore it.
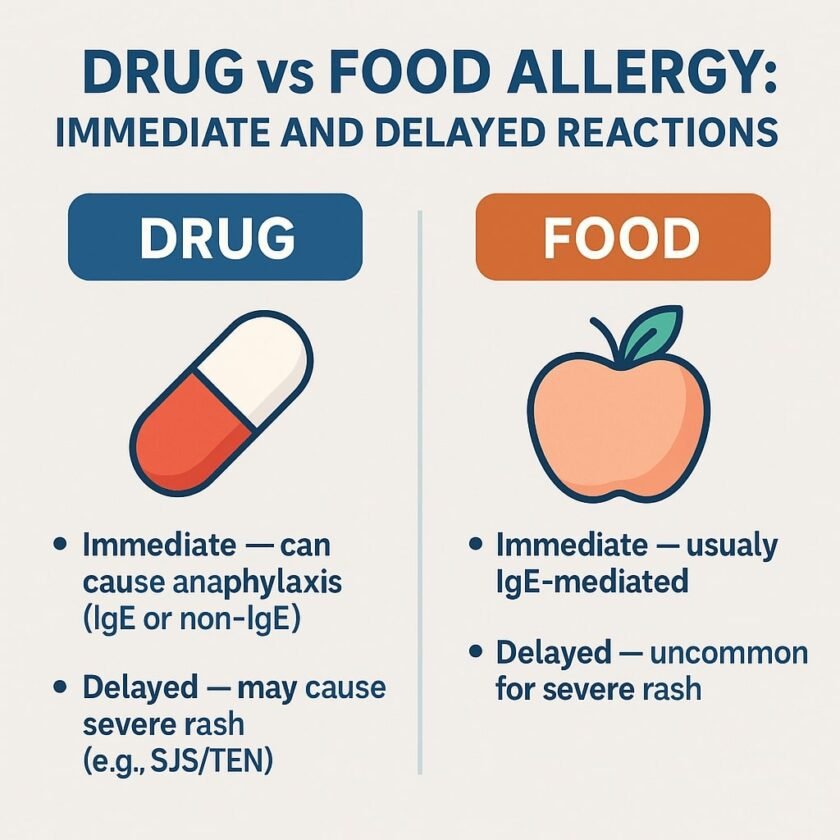
🔍 Summary for General Readers
The immune system must stay in balance—not too weak, not too strong. Two rare genetic conditions show what happens when that balance breaks in opposite directions:
STAT1 Gain-of-Function (GOF): The brake is stuck on. Interferon signals become too strong, making the immune system overactive and eventually burned out, leading to inflammation and infections.
STAT3 Loss-of-Function (LOF): The accelerator is broken. Key defenses, especially those protecting the skin, lungs, and mucous membranes, fail to activate.
Both disorders weaken defense against Candida (yeast), but for different reasons. Understanding their contrast helps guide targeted treatments.
🔬 Understanding These Rare Conditions
Prevalence & Inheritance
Both STAT1 gain-of-function and STAT3 loss-of-function are extremely rare genetic disorders, each estimated to affect fewer than 1 in 1,000,000 people worldwide. However, they may be underdiagnosed due to variable presentation and limited awareness.
Inheritance patterns:
- STAT1 GOF: Autosomal dominant (one mutated copy causes disease)
- STAT3 LOF (AD-HIES): Autosomal dominant (one mutated copy causes disease)
- Some cases arise from new (de novo) mutations with no family history
How Are They Diagnosed?
Diagnosis requires:
- Clinical suspicion based on characteristic infection patterns and associated features
- Genetic testing to identify specific mutations
- Functional immunology studies to assess immune cell function and cytokine responses
- Specialist evaluation by clinical immunologists
Important note: Diagnosis is often delayed by years or decades due to the rarity of these conditions and their variable presentation. Many patients see multiple specialists before the correct diagnosis is made.
🧬 1. Molecular Mechanisms
| Feature | STAT1 Gain-of-Function (GOF) | STAT3 Loss-of-Function (LOF) (AD-HIES / Job’s syndrome) |
| Genetic Effect | Gain-of-function → prolonged STAT1 phosphorylation → delayed deactivation and extended nuclear retention | Loss-of-function → defective STAT3 phosphorylation and transcriptional activation |
| Key Signaling | IFN-α/β, IFN-γ, IL-27 overactive → chronic STAT1 dominance | IL-6, IL-21, IL-23, IL-10, IL-11, IL-22 impaired or nonfunctional |
| IL-10 Response | Impaired (STAT1 interference + SOCS feedback) | Absent (requires STAT3) |
| Impact on STAT3 Programs | STAT1 hyperactivation suppresses STAT3-inducible genes (RORC, IL-17, IL-22, IL-10) | Direct STAT3 loss eliminates these pathways |
| Net Result | Immune overactivation → autoimmunity + paradoxical infections | Immune underactivation → weak mucocutaneous/extracellular defense |
🧩 2. Th17 Pathway & Mucosal Barrier Integrity
| Mechanism | STAT1 GOF | STAT3 LOF |
| Th17 Differentiation | Inhibited by excessive IFN-γ/IL-27 → partial Th17 loss | Intrinsic STAT3 defect → near-complete Th17 developmental failure |
| IL-17 / IL-22 Function | Qualitative impairment: interferon dominance suppresses STAT3-dependent transcription → epithelial dysfunction | Quantitative loss: fewer Th17 cells; innate IL-17 sources (γδ T, ILC3) may partly compensate |
| Fungal Infection (CMC) | Often more severe and chronic with interferon-driven mucosal inflammation (though individual variation is significant) | Usually milder; reduced inflammation can lessen severity |
Key Insight: STAT3 LOF causes a quantitative Th17 deficiency, while STAT1 GOF causes a qualitative IL-17/IL-22 blockade plus interferon-driven tissue injury. This explains why Candida infections can be more severe in STAT1 GOF even when Th17 cells are present.
- Contact the Immune Deficiency Foundation for patient support groups
- Several research centers maintain patient registries for these conditions
🧫 3. Macrophage Function & Intracellular Infections
STAT1 GOF
Chronic IFN-γ signaling creates “hyperinflammatory exhaustion”—macrophages remain activated but functionally blunted.
- ↓ IL-12 production
- Poor granuloma formation
- Impaired killing of intracellular pathogens (e.g., NTM, Salmonella, Histoplasma)
Clinical Implication: Increased susceptibility to mycobacterial and intracellular infections in some patients, though severity varies and is not universal.
STAT3 LOF
The IL-12–IFN-γ–STAT1 axis remains intact, so macrophage killing function is preserved.
Clinical Implication: Mycobacterial infections are rare or absent.
👩⚕️ 4. Clinical Phenotype Comparison
| System / Manifestation | STAT1 GOF | STAT3 LOF (AD-HIES) |
| Infections | Chronic mucocutaneous candidiasis; bacterial & viral infections (HSV, VZV, CMV); variable intracellular infections | Recurrent “cold” Staphylococcus abscesses; bacterial pneumonia with pneumatoceles; Candida usually mild |
| Autoimmunity | Common (thyroiditis, cytopenias, type 1 diabetes) | Rare |
| Connective Tissue / Skeletal | Usually normal | Scoliosis, retained primary teeth, coarse facies, joint hyperextensibility |
| IgE Levels | Normal or mildly ↑ | Markedly ↑ (often >2,000 IU/mL) |
| Eosinophilia | Minimal/absent | Frequent |
| Granulomas | Impaired | Preserved |
| Clinical Pattern | Autoimmunity with infections | Pure immunodeficiency with structural/connective findings |
💊 5. Drug Hypersensitivity & Treatment Considerations
Drug Reaction Patterns in STAT1 GOF vs STAT3 LOF
Understanding these conditions has important implications for medication management. While formal studies on drug hypersensitivity patterns in these specific disorders are limited, the underlying immune dysregulation provides insights into potential risks and considerations.
STAT1 Gain-of-Function: Managing Heightened Inflammatory States
Theoretical Drug Hypersensitivity Considerations:
Based on chronic interferon activation and immune dysregulation, patients with STAT1 GOF may potentially experience:
- Increased inflammatory responses to medications
- More severe cutaneous reactions when the skin barrier is already compromised by chronic inflammation
- Autoimmune-like drug reactions (e.g., drug-induced cytopenias, lupus-like features)
- Altered response to immunomodulatory therapies
Important: These patterns are based on the underlying pathophysiology; systematic studies of drug reactions in STAT1 GOF are still emerging. Individual responses vary significantly.
Treatment Considerations:
JAK Inhibitors (Ruxolitinib, Baricitinib, Tofacitinib)
- Used in selected cases to reduce excessive STAT1 signaling and rebalance STAT3/STAT5 pathways
- Reported benefits in some patients:
- Better control of chronic mucocutaneous candidiasis (CMC)
- Reduction in autoimmune manifestations
- Improved quality of life
- Important safety monitoring required:
- Infections: Increased risk, especially herpes zoster (shingles), bacterial infections
- Cytopenias: Regular monitoring of blood counts (anemia, low platelets, low white cells)
- Liver function: Periodic liver enzyme testing
- Lipids: Monitor cholesterol and triglycerides
- Hypersensitivity reactions: Uncommon but possible; monitor for rash or other allergic symptoms
- Risk-benefit consideration: Given the underlying immunodeficiency, careful patient selection and monitoring are essential
- Not appropriate for all patients: Reserved for those with significant disease burden
Antimicrobial Prophylaxis
- Antifungals (e.g., fluconazole) for recurrent Candida infections
- Antivirals (e.g., acyclovir, valacyclovir) for HSV/VZV when indicated
- Prophylaxis choice depends on individual infection history
Biologic Therapies
- Use with caution: Anti-cytokine therapies must be carefully selected
- Must balance infection risk with potential benefit
- Requires close monitoring
Hematopoietic Stem Cell Transplantation (HSCT)
- Reserved for severe, refractory cases with life-threatening complications
- Outcomes are variable and risks are significant:
- Potential for cure through immune system replacement
- Risks include: graft-versus-host disease, severe infections, treatment-related mortality
- Best outcomes when performed at experienced centers
- Decision requires careful multidisciplinary evaluation
STAT3 Loss-of-Function: Navigating the High-IgE Landscape
Drug Hypersensitivity Profile:
The extremely high IgE levels (often >2,000 IU/mL) in STAT3 LOF require special interpretation:
- High IgE is NON-SPECIFIC in this condition and does NOT automatically indicate true IgE-mediated drug allergy
- Despite sky-high IgE, true IgE-mediated allergies are actually less common than would be expected
- Baseline eosinophilia may increase risk of drug-related eosinophilic reactions
- “Antibiotic reactions” are often reported but frequently represent non-IgE mechanisms (e.g., side effects, viral exanthems, disease flares)
Critical distinction: In STAT3 LOF, high IgE reflects immune dysregulation, not atopy. True allergic reactions remain uncommon.
Treatment Considerations:
Anti-Staphylococcal Prophylaxis (Essential Long-Term)
- Common regimens: TMP-SMX (Bactrim), dicloxacillin, cephalexin
- Why this matters: These antibiotics are often essential for preventing life-threatening infections
- The challenge: Patients may have reported “allergies” to needed antibiotics
- The solution:
- Distinguish true allergy from side effects or disease symptoms
- Formal drug allergy evaluation (skin testing, drug challenge) when needed
- Desensitization protocols available for true allergies to essential medications
- Key principle: Avoiding needed antibiotics may be more dangerous than the perceived allergy
Intravenous Immunoglobulin (IVIg)
- Used when indicated for immune support
- Generally well tolerated
- Rare hypersensitivity reactions possible (mostly related to IgA deficiency, which is uncommon in STAT3 LOF)
Acute Infection Management
- Prompt, appropriate antibiotics are critical
- Skin and lung infections require aggressive treatment
- Early intervention prevents complications (pneumatoceles, abscesses)
Regular Monitoring
- Pulmonary function and chest imaging (pneumatoceles, bronchiectasis)
- Dental surveillance (retained primary teeth, periodontal disease)
- Skeletal monitoring (scoliosis progression)
- Immunology follow-up
Hematopoietic Stem Cell Transplantation (HSCT)
- Considered in severe, life-threatening disease
- Variable outcomes:
- Can be curative in some cases
- Timing of transplant affects outcomes
- Risks include GVHD, infections, and treatment-related complications
- Decision requires careful evaluation of disease severity vs. transplant risks
- Reserved for patients with progressive, refractory disease
🩺 Clinical Pearl: Drug Allergy Testing in These Conditions
When to suspect underlying STAT dysfunction in the drug allergy clinic:
Suspect STAT1 GOF when you see:
- Recurrent or persistent Candida infections (oral, esophageal, genital, skin/nails) + multiple reported drug allergies
- Multiple autoimmune conditions (thyroiditis, cytopenias, type 1 diabetes) + frequent adverse drug reactions
- Unusual infection patterns (viral infections like HSV/VZV; mycobacterial infections) + drug intolerance
Suspect STAT3 LOF when you see:
- Very high IgE (>2,000 IU/mL) + recurrent “cold” staphylococcal abscesses or pneumonias + reported “antibiotic allergies”
- Characteristic features: retained primary teeth (in adults), scoliosis, coarse facial features, recurrent pneumonia + multiple “drug allergies”
- Eczema + severe recurrent infections + extremely high IgE (out of proportion to atopic disease severity)
Drug Allergy Testing Considerations in These Conditions:
Skin Testing Interpretation:
- Baseline immune dysregulation may alter results:
- False positives possible in inflammatory states (STAT1 GOF)
- Non-specific skin reactivity possible
- Requires experienced interpretation
- High IgE in STAT3 LOF:
- Does NOT predict true IgE-mediated drug allergy
- Skin test interpretation same as for other patients
- Positive predictive value may be lower
Drug-Specific IgE Testing:
- Can help differentiate true IgE-mediated allergy from intolerance
- Limited availability for most drugs
- Must be interpreted in clinical context
Drug Challenge/Desensitization:
- Often necessary for essential medications (especially antibiotics in STAT3 LOF)
- Should be performed in appropriate setting with resuscitation available
- Desensitization protocols can enable use of “allergic” drugs when truly needed
Immunology Referral:
- Strongly recommended when STAT dysfunction suspected
- Comprehensive evaluation includes:
- Detailed immunologic testing
- Genetic testing for confirmation
- Coordination with allergy/immunology for drug allergy evaluation
- Long-term management planning
Key Principle for Clinicians: In both conditions, thoroughly evaluate reported “drug allergies.” Many are not true allergies, and avoiding essential medications can be more harmful than the perceived drug reaction. Formal allergy evaluation can clarify true allergies and enable safe use of needed therapies.
⚖️ 6. Conceptual Analogy: “Brake vs. Accelerator”
| Concept | STAT1 GOF | STAT3 LOF |
| Analogy | Brake stuck on | Accelerator broken |
| Immune Dynamics | Over-controlled: interferon dominance suppresses IL-6/IL-23/IL-10/IL-17/IL-22 pathways | Under-activated: failure of differentiation and epithelial repair programs |
| Pathophysiology | Immune exhaustion + autoimmunity with paradoxical infections | Defective Th17 and epithelial repair → immunodeficiency with connective-tissue abnormalities |
| Clinical Outcome | Autoimmunity + fungal/bacterial/viral infections | Extracellular bacterial infections (especially Staph) + structural abnormalities |
| Drug Considerations | Potentially heightened inflammatory responses to medications; JAK inhibitors may help but require careful monitoring | Very high IgE does NOT predict true drug allergy; essential antibiotics often needed long-term despite reported “allergies” |
🧾 7. Summary Table: Key Distinguishing Features
| Feature | STAT1 GOF | STAT3 LOF (AD-HIES) |
| Primary Defect | Hypermorphic STAT1 activation (prolonged signaling) | Hypomorphic or null STAT3 activity |
| Dominant Cytokines | Type I/II interferons (IFN-α/β/γ), IL-27 | IL-6 family (IL-6, IL-21, IL-23, IL-11, IL-22) |
| Th17 Impairment | Qualitative IL-17/IL-22 blockade (via STAT1 suppression of STAT3 programs) | Quantitative failure of Th17 development |
| Candida Infection (CMC) | Often severe and chronic (though variable) | Usually mild or absent |
| Mycobacterial Risk | Increased in some patients (macrophage dysfunction) | Low (intact IFN-γ–STAT1 axis) |
| Autoimmunity | Prominent (thyroiditis, cytopenias, diabetes, others) | Rare |
| Skeletal/Connective | Usually absent | Characteristic (scoliosis, retained teeth, coarse facies, hyperextensibility) |
| IgE Level | Normal to mildly elevated | Markedly elevated (often >2,000 IU/mL) |
| Eosinophilia | Minimal or absent | Common |
| Drug Considerations | Potentially increased inflammatory-type reactions; caution with immunosuppression | High IgE ≠ high allergy risk; distinguish true allergy from side effects for essential antibiotics |
| Key Management | JAK inhibitors in selected cases ± antimicrobial prophylaxis ± immunomodulation | Long-term anti-staphylococcal prophylaxis ± IVIg; aggressive infection treatment |
| HSCT | Reserved for severe, refractory disease; variable outcomes | Considered for life-threatening disease; timing and patient selection crucial |
🌐 8. Integrative Perspective & Clinical Takeaway
STAT1 GOF: Too Much Signal, Too Little Control
Interferon dominance drives chronic inflammation while paradoxically suppressing protective STAT3-dependent pathways. This creates a unique situation where the immune system is simultaneously overactive (causing autoimmunity and tissue inflammation) and underperforming (allowing infections to persist).
Clinical implications:
- Infections occur despite an “activated” immune system
- Autoimmunity may complicate the clinical picture
- Drug responses may be unpredictable due to baseline inflammation
- Some patients benefit from targeted therapy with JAK inhibitors, which can help restore balance
STAT3 LOF: Too Little Signal, Too Weak Defense
Loss of STAT3-dependent helper and repair programs creates a specific vulnerability: defective mucosal and epithelial defenses, particularly against extracellular bacteria like Staphylococcus aureus. The connective tissue abnormalities add another dimension to this syndrome.
Clinical implications:
- The very high IgE is a red herring—it doesn’t predict allergic disease
- Structural problems (teeth, bones, lungs) are as important as infections
- Long-term antibiotic prophylaxis is often essential
- True drug allergies must be distinguished from reported reactions to enable appropriate care
Precision Medicine: The Promise and the Challenges
Targeted therapies like JAK inhibitors represent a paradigm shift in managing STAT1 GOF, moving from treating symptoms to addressing the molecular defect. However:
- Not all patients respond equally
- Significant monitoring is required
- Infection risk remains a concern
- Long-term outcomes are still being studied
For both conditions, the goal is to work with the dysregulated immune system rather than against it—supporting what’s weak, calming what’s overactive, and carefully selecting medications that help rather than harm.
The Balance Between Protection and Tolerance
These two rare conditions teach us fundamental lessons about immune balance:
- Too much signal (STAT1 GOF) is as problematic as too little (STAT3 LOF)
- The immune system needs both activation and restraint
- Context matters: The same cytokine pathways that fight infections also maintain tissue integrity and prevent autoimmunity
- Drug responses depend on immune context: Understanding the underlying immune state helps predict and manage medication reactions
When the immune system’s rhythm falters, everything downstream changes—from fighting infections to tolerating medications. These conditions remind us that immune health isn’t about being “strong” or “weak,” but about being balanced and adaptable.
🚨 When to Consult a Specialist
Consider immunology referral if you or your patient experiences:
Red Flags for STAT1 GOF:
- Chronic or recurrent mucocutaneous candidiasis (oral, esophageal, genital, nail infections) resistant to standard treatment
- Multiple autoimmune conditions, especially with unusual infections
- Recurrent viral infections (HSV, VZV) + fungal infections + possible mycobacterial infections
- Family history of similar unusual infection patterns
Red Flags for STAT3 LOF (Hyper-IgE Syndrome):
- Extremely high IgE (>2,000 IU/mL) + recurrent skin abscesses + pneumonia with pneumatoceles
- Retained primary teeth in teenagers/adults + recurrent infections
- Eczema + severe infections + skeletal abnormalities (scoliosis, fractures)
- “Cold” abscesses (not red, hot, or particularly painful despite size)
Drug Allergy Considerations Warranting Evaluation:
- Multiple reported “drug allergies” in a patient with unusual or severe infections
- Need for long-term prophylactic antibiotics but reported “allergies” to first-line options
- Adverse drug reactions that seem disproportionate or unusual
- Difficulty finding tolerated medications in a patient with complex immunodeficiency
Why Drug-Allergy Evaluation is Critical in These Conditions:
- These patients often NEED specific medications long-term
- Antibiotics for prophylaxis (STAT3 LOF)
- Antifungals for chronic candidiasis (STAT1 GOF)
- JAK inhibitors for immune modulation (selected STAT1 GOF cases)
- True allergies must be distinguished from:
- Side effects (e.g., GI upset, headache)
- Disease-related symptoms (e.g., rash from viral infection)
- Non-IgE mediated reactions that may not recur
- Desensitization protocols are available
- Can enable use of “allergic” medications when truly essential
- Should be performed in appropriate setting by experienced providers
- Avoiding needed medications can be more dangerous
- Untreated infections can be life-threatening
- Suboptimal antibiotic choices increase resistance risk
- Delayed treatment worsens outcomes
What to Expect from Specialist Evaluation:
Immunology Assessment:
- Detailed infection and autoimmune history
- Comprehensive immune testing (lymphocyte subsets, cytokine responses, antibody levels)
- Genetic testing for STAT1/STAT3 mutations
- Family history evaluation
Allergy/Immunology Collaboration:
- Review of all reported drug reactions
- Determination of which reactions warrant formal testing
- Skin testing when appropriate
- Drug challenge or desensitization when indicated
- Long-term medication management planning
Multidisciplinary Care:
- Infectious disease (for complex infection management)
- Pulmonology (for lung complications, especially in STAT3 LOF)
- Rheumatology (for autoimmune manifestations in STAT1 GOF)
- Dentistry (for dental complications in STAT3 LOF)
- Orthopedics (for skeletal issues in STAT3 LOF)
📚 References & Further Reading
This article integrates findings from major cohort studies and clinical reviews on STAT1 and STAT3 signaling disorders. While the molecular mechanisms and clinical features are well-established, formal studies on drug hypersensitivity patterns in these specific conditions remain limited. The drug reaction considerations presented here are based on underlying pathophysiology and clinical experience.
For healthcare providers: Always consult current primary literature and specialty guidelines when making clinical decisions. Management of these complex disorders should be personalized and conducted in collaboration with clinical immunology specialists.
For patients and families: This information is educational and should not replace consultation with your healthcare providers. Individual presentations vary significantly, and treatment plans should be tailored to your specific situation.
Last Updated: October 2025
📚 Suggested Readings: STAT1 GOF vs. STAT3 LOF
About these resources: The following readings are organized by audience and topic. All citations follow Vancouver style with embedded hyperlinks for easy access. Open-access articles are noted where available.
👨👩👧 For Patients and Families
1 🏥 Immune Deficiency Foundation. STAT1 and STAT3 Gain of Function [Internet]. Towson (MD): Immune Deficiency Foundation; [cited 2025 Oct 18].
Free resource – Patient-friendly overview
2 🏥 Immune Deficiency Foundation. Hyper IgE Syndrome [Internet]. Towson (MD): Immune Deficiency Foundation; [cited 2025 Oct 18].
Free resource – Patient-friendly overview
3 📖 Hsu AP, Davis J, Puck JM, Holland SM, Freeman AF. STAT3 Hyper IgE Syndrome. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2025 [updated 2020 Mar 26].
Free full text – Comprehensive but technical
4 🏥 National Organization for Rare Disorders. Autosomal Dominant Hyper IgE Syndrome [Internet]. Danbury (CT): NORD; [cited 2025 Oct 18].
Free resource – Overview of STAT3 LOF/HIES
🔬 Foundational Scientific Papers
5 📄 Liu L, Okada S, Kong XF, Kreins AY, Cypowyj S, Abhyankar A, et al. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J Exp Med. 2011;208(8):1635-48.
First description of STAT1 GOF mechanism
6 📄 Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Brodsky N, et al. STAT3 mutations in the hyper-IgE syndrome. N Engl J Med. 2007;357(16):1608-19.
Landmark identification of STAT3 mutations in HIES
7 📄 Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, et al. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 2007;448(7157):1058-62.
Original STAT3 mutation discovery
👩⚕️ Major Cohort Studies & Clinical Reviews
8 📊 Toubiana J, Okada S, Hiller J, Oleastro M, Lagos Gomez M, Aldave Becerra JC, et al. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood. 2016;127(25):3154-64.
Largest international cohort (274 patients) – Essential reading
9 📊 Zhang W, Chen X, Gao G, Xing L, Wen L, Mo Y, et al. Clinical Relevance of Gain- and Loss-of-Function Germline Mutations in STAT1: A Systematic Review. Front Immunol. 2021;12:654406.
Open access – Systematic review of 442 STAT1 GOF patients
10 📊 Tsilifis C, Freeman AF, Gennery AR. STAT3 Hyper-IgE Syndrome—an Update and Unanswered Questions. J Clin Immunol. 2021;41(5):864-80.
Recent comprehensive update on STAT3 LOF
💊 Treatment: JAK Inhibitors and Management
11 💉 Higgins E, Al Shehri T, McAleer MA, Conlon N, Feighery C, Lilic D, et al. Use of ruxolitinib to successfully treat chronic mucocutaneous candidiasis caused by gain-of-function signal transducer and activator of transcription 1 (STAT1) mutation. J Allergy Clin Immunol. 2015;135(2):551-3.e3.
First report of JAK inhibitor use in STAT1 GOF
12 💉 Deyà-Martínez À, Rivière JG, Roxo-Junior P, Ozsurekci Y, Bonnet C, Lévy R, et al. Impact of JAK Inhibitors in Pediatric Patients with STAT1 Gain of Function (GOF) Mutations—10 Children and Review of the Literature. J Clin Immunol. 2022;42(5):1071-82.
Pediatric experience with JAK inhibitors
13 💉 Flanagan SE, Haapaniemi E, Russell MA, Caswell R, Lango Allen H, De Franco E, et al. Emerging Place of JAK Inhibitors in the Treatment of Inborn Errors of Immunity. Front Immunol. 2021;12:717388.
Open access – Comprehensive JAK inhibitor review
🩺 Drug Hypersensitivity in Primary Immunodeficiency
14 ⚕️ Ponsford MJ, Klocperk A, Pulvirenti F, Dalm VASH, Milito C, Cinetto F, et al. Hyper-IgE in the allergy clinic—when is it primary immunodeficiency? Allergy. 2018;73(11):2122-36.
Essential for distinguishing PID from allergy
15 ⚕️ Chan SK, Hanson IC. Primary immunodeficiency masquerading as allergic disease. Immunol Allergy Clin North Am. 2015;35(4):767-78.
PID presenting with allergic symptoms
📌 Access Note: Some articles may require institutional access or purchase. Many university libraries and hospitals provide access to these journals. If you cannot access a paper, contact your local medical library or the corresponding author—many researchers are happy to share their work.