Recent advances in immunology have deepened our understanding of allergic diseases and hypersensitivity reactions. Traditionally classified using the Gell-Coombs system (Types I-IV), the increasing complexity of these conditions has led to a proposed new nomenclature, especially for Type IV hypersensitivity. This blog provides an overview of the new classification and its clinical implications.
Overview of Traditional Hypersensitivity Classification
The Gell-Coombs classification includes:
Type I Hypersensitivity: Immediate reactions mediated by IgE, causing conditions like anaphylaxis, allergic rhinitis, and asthma.
Type II Hypersensitivity: Cytotoxic reactions involving IgG or IgM antibodies, leading to diseases like hemolytic anemia.
Type III Hypersensitivity: Immune complex-mediated reactions, seen in conditions like systemic lupus erythematosus.
Type IV Hypersensitivity: Delayed-type reactions mediated by T cells, subdivided into Type IVa (monocyte/macrophage), IVb (eosinophil/Th2), IVc (cytotoxic T cell), and IVd (neutrophil).
Here are the novel classifications of hypersensitivity reactions according to the new European Academy of Allergy and Clinical Immunology Position Paper published in Allergy. 2023 Nov;78(11):2851-2874. and Allergy. 2024 Jan;79(1):269-273.
Type I Hypersensitivity (Immediate) – IgE-Mediated Response
- Mechanism: Sensitization by allergens leads to IgE production by B cells. Upon re-exposure, allergens crosslink IgE on mast cells, triggering degranulation and release of inflammatory mediators (histamine, leukotrienes).
- Clinical Manifestations: Allergic rhinitis, asthma, eczema, food allergies, anaphylaxis.
Type II Hypersensitivity (Antibody-Mediated Cytotoxicity) – Drug-Induced Reactions
- Mechanism: Antibodies target and destroy cells coated with drugs or their metabolites. This can occur through complement activation, immune cell cytotoxicity, or phagocytosis.
- Clinical Manifestations: Drug-induced cytopenias (low blood cell counts), autoimmune diseases like hemolytic anemia.
Type III Hypersensitivity (Immune Complex-Mediated) – Antigen-Antibody Complexes
- Mechanism: Soluble antigen-antibody complexes form and deposit in tissues, activating complement and attracting inflammatory cells, leading to tissue damage.
- Clinical Manifestations: Serum sickness, vasculitis, glomerulonephritis (kidney inflammation).
New Nomenclature for Type IV Hypersensitivity
The new nomenclature consolidates Type IV hypersensitivity into three primary types:
Type IVa – T1 Immune Response
Type IVb – T2 Immune Response
Type IVc – T3 Immune Response
Each type has distinct immune mechanisms and clinical manifestations.
Type IVa Hypersensitivity – T1 Immune Response
-
- Mechanism: Mediated by Th1 and Tc1 cells, producing IFN-γ and engaging in cytotoxic activities.
-
- Clinical Manifestations: Conditions include allergic contact dermatitis, celiac disease, non-T2 endotypes of asthma, and non-immediate drug allergies.
-
- Key Players: Th1 cells, Tc1 cells, IFN-γ, TNF-α.
Type IVb Hypersensitivity – T2 Immune Response
-
- Mechanism: Involves Th2 cells, producing cytokines like IL-4, IL-5, IL-9, and IL-13, crucial for IgE class switching and eosinophil recruitment.
-
- Clinical Manifestations: Conditions include T2 endotype asthma, allergic rhinitis, atopic dermatitis, and food allergies.
-
- Key Players: Th2 cells, IL-4, IL-5, IL-13, eosinophils.
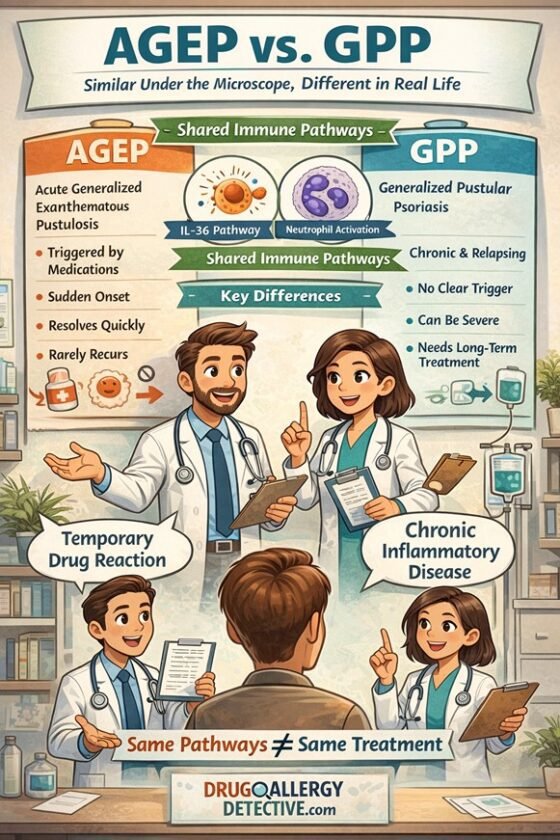
Type IVc Hypersensitivity – T3 Immune Response
-
- Mechanism: Mediated by Th17 cells and other IL-17-producing cells, promoting neutrophil recruitment.
-
- Clinical Manifestations: Conditions include neutrophilic asthma and psoriasis.
-
- Key Players: Th17 cells, IL-17A, IL-17F.
Other Potential Types of Type IV Hypersensitivity
Pharmacological Interaction with Immune Receptors (p-i Concept)
-
- Mechanism: Drugs directly bind to T-cell receptors or HLA molecules, stimulating immune cells without antigen processing.
-
- Clinical Manifestations: Conditions like Stevens-Johnson syndrome and toxic epidermal necrolysis.
Th9 and Th22 Cell-Mediated Responses
-
- Mechanism: Th9 cells produce IL-9, influencing allergic inflammation; Th22 cells secrete IL-22, targeting epithelial cells.
-
- Clinical Manifestations: Th9 cells are linked to asthma; Th22 cells play a role in atopic dermatitis.
Type V Hypersensitivity- Epithelial Barrier Defect
- Mechanism: Weak barrier allows allergens and irritants in, triggering immune response.
- Clinical Manifestations: Chronic inflammatory conditions like eczema, asthma, and food allergies.
Type VI Hypersensitivity – Metabolic-induced Immune Dysregulation
- Mechanism: Obesity/metabolic issues cause inflammation and gut microbiome changes, increasing allergy risk.
- Clinical Manifestations: Increased risk of asthma, especially in obese individuals; worsened allergies.
Type VII Hypersensitivity – Direct Cellular and Inflammatory Response to Chemical Substances
- Mechanism: Certain drugs/chemicals directly activate immune cells, causing allergic reactions.
- Clinical Manifestations: Idiosyncratic reactions to medications (NSAIDs) leading to asthma, urticaria, or angioedema.
Our Perspectives on this research
Implications for Clinical Practice
The new classification system provides a more nuanced understanding of immunological mechanisms, aiding in improved diagnostic accuracy, targeted treatments, and personalized therapeutic approaches. Treatment strategies can be tailored to the specific immune pathways involved in each hypersensitivity subtype:
-
- Type IVa: Corticosteroids, immunosuppressive drugs, anti-IFN-γ antibodies.
-
- Type IVb: Anti-IL-4 and anti-IL-13 biologics, treatments for eosinophilic inflammation.
-
- Type IVc: IL-17 pathway-targeting biologics.
Merging Type IVa and IVc
The new nomenclature merges Type IVa and IVc hypersensitivity into Type IVa, encompassing a broader range of conditions. However, the classification’s stance on drug-induced conditions like Stevens-Johnson syndrome remains unclear.
Uncertain Placement of Peculiar Reactions
The classification does not definitively categorize reactions like cytokine release syndrome or complement-related pseudoallergy, suggesting the need for a separate category.
Challenges and Future Directions
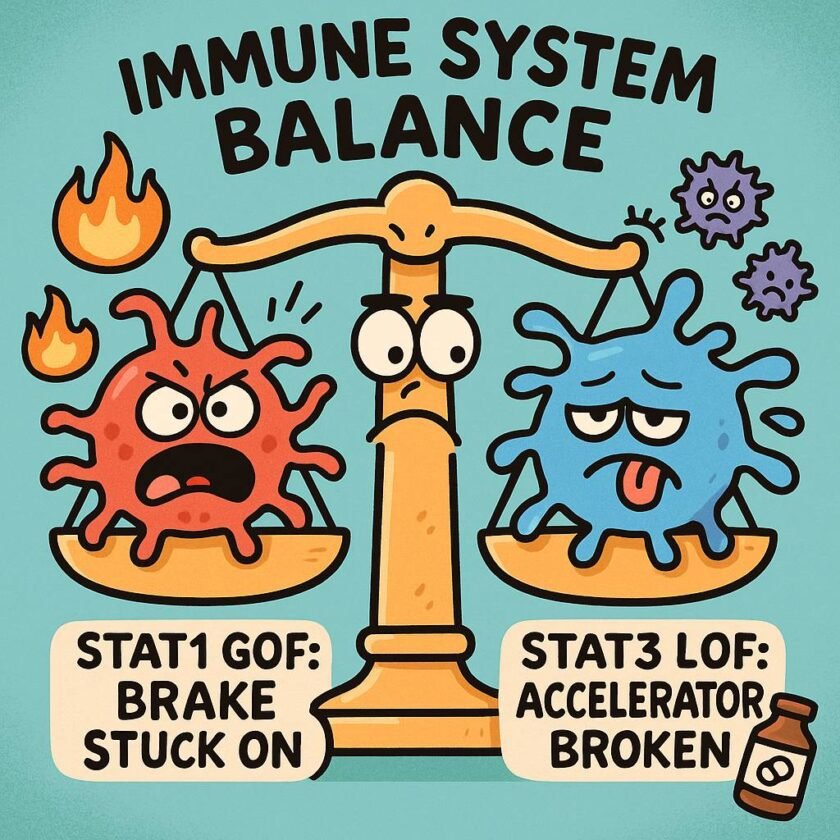
Multiple immune responses can occur simultaneously, complicating subtype distinctions. Despite this, the new nomenclature enhances our understanding of allergic reactions, paving the way for more specific and effective therapies, ultimately improving patient care.
References