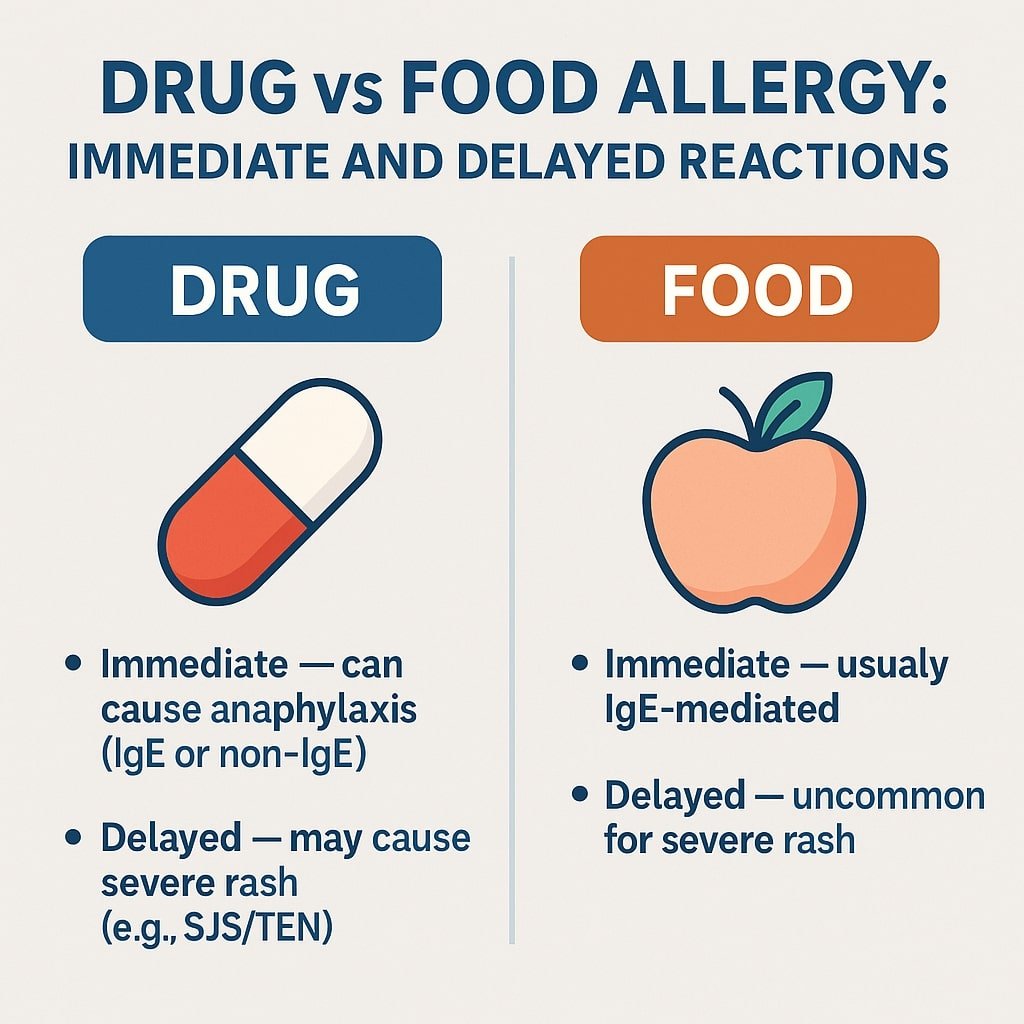
Drug vs Food Allergy: Why Medications Can Cause Both Immediate and Delayed Reactions — While Foods Uncommonly Cause Severe Delayed Reactions
This article is for educational purposes only. Always consult healthcare providers for personalized medical advice.
Patients often ask:
“Why can medications cause both rapid allergic reactions like hives or anaphylaxis and dangerous delayed reactions such as Stevens–Johnson Syndrome (SJS) or Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), while food allergies almost always appear immediately?”
The difference lies in how the immune system processes drugs versus foods — and in the unique ways small drug molecules can interact with immune receptors.
🩺 Quick Summary
Drugs can cause:
- Immediate reactions: Anaphylaxis (IgE-mediated or non-IgE via MRGPRX2).
- Delayed reactions: Simple rashes or severe T-cell–mediated syndromes such as SJS/TEN and DRESS.
- Mechanisms: Hapten/pro-hapten for some reactions, but also PI concept and altered peptide repertoire model for severe cutaneous adverse reactions (SCARs).
Foods usually cause:
- Immediate IgE-mediated reactions, but non-immediate reactions do occur (e.g., fixed food eruption, FPIES, severe reactions to certain herbal/traditional medicines).
- Severe delayed skin reactions (like SJS/TEN and DRESS) are overwhelmingly drug-induced, although infections and herbal remedies can occasionally mimic them.
How the Immune System “Sees” Drugs vs Foods
Drugs: Small Molecules With Multiple Immune Pathways
Consider two patients:
- One develops hives 30 minutes after taking amoxicillin → an immediate, likely IgE-mediated reaction.
- Another develops a severe rash 2 weeks after starting carbamazepine → a delayed, T-cell–mediated reaction.
These differences highlight why timing is so important for diagnosis.
Immediate Reactions (minutes–hours)
- IgE-mediated anaphylaxis: Classic allergic pathway. IgE antibodies bind to a drug; on re-exposure, mast cells release histamine → hives, swelling, wheezing, anaphylaxis.
- Common culprits: beta-lactam antibiotics (penicillins, cephalosporins), some platinum chemotherapies.
- Non-IgE-mediated anaphylaxis: Some drugs directly activate mast cells via the MRGPRX2 receptor. This explains why some patients can have severe reactions to a drug they’ve never taken before.
- Examples: NMBAs, fluoroquinolones, radiocontrast media, opioids.
Delayed Reactions (days–weeks)
While the hapten/pro-hapten model explains many simple drug rashes, severe reactions like SJS/TEN and DRESS are better explained by newer models:
- PI Concept (Pharmacological Interaction with Immune Receptors):
Drugs can bind directly and reversibly to HLA molecules or T-cell receptors (TCRs) without prior processing. This triggers powerful T-cell responses and explains why risk is tied to certain HLA alleles.- Examples: Carbamazepine-induced SJS/TEN in HLA-B15:02 carriers; Allopurinol-induced SCARs in HLA-B58:01 carriers.
- Altered Peptide Repertoire Model:
Drugs fit inside the HLA binding groove, changing which peptides are displayed. Normal “self-peptides” may then look foreign → massive cytotoxic T-cell activation.- Example: Abacavir hypersensitivity in HLA-B*57:01 carriers.
Foods: Complete Proteins With an IgE Bias (but not exclusively)
Food allergens are usually proteins or glycoproteins (10–70 kDa). In the gut, they are processed in a Th2-biased immune environment that favors IgE production.
- On re-exposure, IgE cross-links on mast cells → rapid release of histamine → symptoms like hives, swelling, wheezing, anaphylaxis (usually within minutes to 2 hours).
Non-Immediate Food Reactions (Important Exceptions)
- Fixed Food Eruption (FFE): Recurrent rash in the same location after a food, similar to fixed drug eruption.
- FPIES (Food Protein-Induced Enterocolitis Syndrome): Non-IgE reaction in infants → delayed vomiting and lethargy 2–6 hours after ingestion.
- Allergic proctocolitis and celiac disease: Chronic, T-cell–mediated conditions.
- Herbal/traditional medicines: Complex mixtures may provoke severe immune-mediated rashes, occasionally resembling SCARs.
Key Point: While foods can cause non-immediate reactions, life-threatening SCARs (SJS/TEN, DRESS) are overwhelmingly linked to drugs.
🧭 Practical Diagnostic Framework
Minutes–2 hours after exposure
- Consider: food allergy (IgE-mediated), drug anaphylaxis (IgE or MRGPRX2), or cofactor-dependent food reactions (e.g., exercise, NSAIDs, alcohol).
- Don’t forget additives (sulfites, benzoates) or scombroid (histamine fish poisoning).
- Always ask: Were any medications, supplements, or herbal products taken at the same time?
4–28 days after starting a drug
- Strong indicator of T-cell–mediated drug reactions such as MPE, DRESS, SJS/TEN.
- Review all drugs taken in the past 1–8 weeks, even intermittent or topical.
✅ Take-Home Messages
- Drugs can cause both immediate (IgE or non-IgE) and delayed (T-cell mediated) allergic reactions.
- Severe delayed reactions (SJS/TEN, DRESS) are best explained by the PI and altered peptide models, often tied to specific HLA risk alleles.
- Foods usually trigger immediate IgE-mediated reactions, but exceptions exist (FFE, FPIES, herbal reactions).
- SCARs are predominantly drug-induced, though infections and herbal medicines can occasionally mimic.
- Accurate diagnosis and safe management should always involve an allergy specialist.
🔎 FAQ
Can drugs cause anaphylaxis without IgE?
Yes. Certain drugs (e.g., NMBAs, fluoroquinolones) activate mast cells via MRGPRX2, bypassing IgE.
Do all delayed drug reactions use the hapten mechanism?
No. SJS/TEN and DRESS are better explained by the PI concept and altered peptide repertoire model.
Can foods cause delayed rashes?
Yes. Fixed food eruption and FPIES are examples. But foods very rarely cause severe delayed syndromes like SJS/TEN.
Why are HLA types important in drug allergy?
Certain HLA alleles (e.g., HLA-B15:02, HLA-B58:01, HLA-B*57:01) strongly predispose to SCARs through direct drug–HLA–TCR interactions.
References
2. McNeil BD. MRGPRX2 and adverse drug reactions. Frontiers in immunology. 2021 Aug 6;12:676354.